Tissue valves (also called biologic or bioprosthetic valves) are made of human or animal tissue. Some valves may have some artificial parts to help give the valve support and to aid placement.
There are three types of tissue valves: pig tissue (porcine), cow tissue (bovine), and human (allografts or homografts).
Porcine stented valve

Information and photographs posted with permission from Edwards Lifesciences®
The porcine stented valve was the first generation of porcine tissue valves. They have been available for more than 30 years.
The valves are made from natural porcine aortic valves, but may be used for aortic or mitral valve replacement. They are trimmed and then fixed in buffered glutaraldehyde at high pressure. The valves are mounted on flexible stents (frames). The bottom of the valve is covered with a seamless knitted polytetrafluoroethylene cloth. This material helps to facilitate the healing and ingrowth of tissue around the implanted valve.
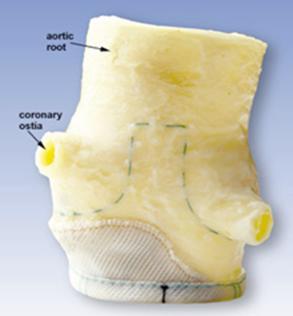
Porcine stentless valve
Information and photographs posted with permission from Edwards Lifesciences®
The porcine stentless valve is used for aortic valve replacement. The valve is made from a natural porcine aortic valve and is fixed in buffered glutaraldehyde solution at a low pressure.
No stents or synthetic sewing rings are used. Therefore, these valves are very similar to the homograft valve (see below).
These valves are technically more difficult to implant but are useful in patients with small hypertrophied hearts.
The Carpentier-Edwards PERIMOUNT Pericardial Bioprosthesis

Information and photographs posted with permission from Edwards Lifesciences®
Valves built to last
Heart valves are marvels of natural engineering. Most people's last a lifetime. But when valves go bad, they may need to be repaired or replaced. Almost 90,000*1 Americans a year need surgery for valve disease. Many of these people will get new, replacement valves made of mechanical or biologic (animal) materials. Which type of valve they get is an important decision and is often not decided until the time of surgery.
Up until now, the biologic valve had one big disadvantage: it didn't last very long. The valve was made of bovine pericardial tissue (tissue from a cow heart) that has been preserved in a buffered glutaraldehyde solution and mounted on a flexible frame and a sewing ring of molded silicone rubber, which allows the surgeon to sew the valve to the patient. Both the frame and the sewing ring are covered with a knitted polytetrafluoroethylene (PTFE) cloth.
The aortic pericardial bioprosthesis has been implanted internationally since 1981, and in the United States since 1991. In the summer of 2000, Carpentier-Edwards released a PERIMOUNT valve for the mitral position.
The benefit of this valve is enhanced durability, which is related to the use of pericardium and the specific bioengineering involved in the valve design.
Recently, however, Cleveland Clinic Heart Center researchers have turned that belief on its head. The biologic valve turns out to be a lot tougher than many people thought.
Mechanical valves are known to be very sturdy. They are made of carbon covered with polyester mesh, and are practically indestructible. The big drawback is that patients who get this type of valve also need to take special blood thinners for the rest of their lives. Biological valves, by contrast, are made of specially processed and shaped animal tissue. They don't require the patient to take the blood thinners forever (unless they have other conditions which warrant it). On the other hand, surgeons were hesitant to implant them in patients who were much younger than 60. It was thought that they would wear out long before the patient did.
That belief has now been challenged. Heart Center researchers Michael Banbury, M.D., Delos Cosgrove, M.D., James Thomas, M.D., and others2, discovered that patients who had received biologic heart valves, did very well. Even 17 years later.
The Heart Center researchers studied 267 patients who had received a Carpentier-Edwards aortic pericardial valve replacement between 1981 and 1983. The researchers followed up on these patients every year thereafter. Many patients not only got echocardiograms, they filled out questionnaires. Outcome measurements included improvements or declines in the New York Heart Association classification of clinical symptoms and echo measurements to determine performance of the valve and size of the valve opening.
How did they do? According to Dr. Banbury, (Cleveland Clinic Heart Center, Department of Cardiovascular Surgery) after 17 years they were doing very well. The majority of patients, even with an increasing age enjoyed good functional status.
"The hemodynamic durability of this valve is excellent and resilient over time," says Dr. Banbury. "The findings from this study support its use in patients and may be considered for individuals younger than 65 years."
(Banbury MK, Cosgrove DM 3rd, Thomas JD, Blackstone EH, Rajeswaran J, Okies JE, Frater RM. Hemodynamic stability during 17 years of the Carpentier-Edwards aortic pericardial bioprosthesis. Ann Thorac Surg. 2002 May;73(5):1460-5)
Aortic Valve Allograft - the Homograft Valve

Information and photographs posted with permission from CryoLife®, Inc
A homograft (also called allograft) is a valve that has been removed from a donated human heart, preserved and frozen under sterile conditions.
Homografts are ideal valves for aortic valve replacement, especially when the aortic root is diseased or there is infection. The heart's natural anatomy is preserved and patients do not need to be on any blood-thinner medications. Although the limited availability is a drawback in some settings, we maintain a large supply.
Ross Procedure
The Ross procedure involves switching your pulmonary valve to the aortic valve position and then placing a pulmonary homograft. This is a very complex procedure; however it has many benefits, especially for young patients with aortic valve disease. Techniques, such as the Ross Procedure are examples of innovative ways surgeons are able to treat valve disease while protecting the heart's natural functioning.
The Ross operation is usually performed on patients younger than ages 40 to 50 who want to avoid taking the blood-thinning medication, Coumadin, after surgery. During this procedure, the patient's normal pulmonary valve is removed and used to replace the diseased aortic valve. The pulmonary valve is then replaced with a pulmonary homograft. The immediate success rate in the operating room is very good, which means that most of the patients intended to have a Ross operation do leave the operating room with a successfully completed Ross operation and well-functioning valves.
The Ross operation is not performed when operative findings contraindicate the procedure, or when the pulmonary valve does not appear normal on the echocardiogram or on inspection. The procedure may also be abandoned when any other technical issues are present.
Advantages: The pulmonic valve is anatomically very similar to the aortic valve and could be an ideal substitute for the aortic valve. The new aortic autograft is a living valve and it will grow as the child or adolescent grows, making this a good option for young patients. The blood flows with less pressure through the pulmonary valve than the aortic valve, therefore a homograft valve could last longer in the right-sided pulmonary valve position. The risk of thromboembolic complications (blood clots, stroke) and the risk of valve infection is very low, lower than for any alternative valve prosthesis. The hemodynamic performance makes the Ross operation an attractive alternative for athletes. The pulmonary autograft valve has a good chance of being a life-lasting solution for the aortic valve. Our qualified guess is that this is going to be the case in 50% of Ross procedure patients.
Drawbacks: The Ross procedure is a technically difficult and long surgery, as it requires two valve replacements. Therefore, this procedure is only recommended for young patients who would tolerate a long surgery time. The pulmonary autograft valve is transplanted from the low pressure pulmonary circulation over to the aortic high pressure system. The valve cusps are strong enough to withstand the systemic pressure, but the pulmonary artery wall does dilate when exposed to systemic pressure, occasionally enough to cause the autograft valve to leak. The risk of requiring re-operation for a leaking autograft valve is about 10 percent within 10 years after the operation. The Ross procedure is not recommended for patients with tissue defects (such as Marfan syndrome) or for patients who have an abnormal pulmonary valve. The pulmonary homograft in the pulmonary position could also fail; the most common mode of failure is that it becomes stenotic. The risk of requiring replacement of the pulmonary homograft is about 10 percent 10 years after the procedure.
The Ross procedure should only be performed by very skilled and experienced surgeons, particularly interested in the operation.
Who makes the final decision?
Choosing the best surgery for you requires a frank and open conversation with your physician regarding your own personal risks and benefits for each surgical option. Then, you and your cardiologist should choose the best surgeon to perform the operation. The surgeon should have experience in performing the procedure and good surgical outcomes. The final decision is made by the surgeon, and this may not occur until the surgery itself, when the surgeon is able to view the diseased valve.
There are advantages and drawbacks to biologic valves.
Advantages: Most patients do not need to be on lifelong blood-thinner medication, unless they have other conditions (such as atrial fibrillation) which warrant it.
Drawbacks: Biologic valves, traditionally, were not considered as durable as mechanical valves, especially in younger people. Previously available biologic valves usually needed to be re-replaced after about 10 years However, recent studies on the PERIMOUNT aortic valve, show that these valves may last at least 17 years without decline in function. This represents a new milestone in durability of biologic valves.
The decision whether to choose a bioprosthetic or a mechanical valve is based on patient choice. In younger patients, the patient may weigh the inconvenience of taking a blood thinner (warfarin) versus the possibility of reoperation during their lifetime. In patients more than 60 years of age, the bovine pericardial valve will probably last for the duration of the patient's life.
